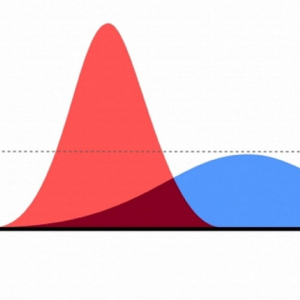
Slogans such as “this viral pandemic respects no borders” or “this is an equal opportunity virus” are often echoed across media platforms and by officials. However, the true impact of pandemics like COVID-19 is rarely homogenous. The spread of the disease and its outcomes affect different persons in different circumstances and at different times in various ways. The interplay between the pathogen, host and the environment shapes transmission dynamics. This granularity is key to understanding and designing appropriate and targeted measures to mitigate epidemics and this pandemic.
Whilst migrants are a heterogenous group, some may be at greater risk of acquisition and transmission of COVID-19 through several factors or trajectories. Consider these 4 reasons.
Reason #1
Precarious working and cramped living conditions may place migrant workers, including those that are low-waged, at higher risk. The resurgence of viral transmission in some countries has been attributed to the lack of effective policies and practices in ensuring protections to low-waged workers. In Singapore for instance, the Ministry of Health reported the largest number of new cases in the "second wave" of COVID19 infections to be linked to such migrant workers residing in dormitory side accomodation.
Reason #2
If entitlements or access to health care is restricted within domestic legal and policy frameworks, this may augment transmission risks, adverse outcomes and inhibit access to early detection, treatment and public health management. Migrants are often excluded from national pandemic plans. A 2018 study on pandemic influenza plans in the Asia Pacific region showed that only a few countries have meaningfully included non-citizens.
Reason #3
(Abrupt) restrictions on travel and border closures without adequate protections and support can lead to mass exodus of migrant worker populations (both internal and international) which may increase health vulnerabilities.
Reason #4
The pandemic has devastated livelihoods of many migrant workers globally. Migrants typically send money back to their families at home; these remittances can boost living standards in poorer countries, such as south Asia, sub-Saharan Africa and South America. Remittances improve global health by improving nutrition and education and reduce child labour. According to the World Bank, the economic crisis induced by COVID-19 could have a negative impact on remittances; In 2020, remittance flows to low- and middle-income countries are expected to drop by around 20 percent to USD445 billion, from USD554 billion in 2019. Europe and Central Asia is estimated to be among the hardest hit regions by this decrease of remittances.
Including migrants in crises and response plans
It is worth considering migrants at every stage of the epidemic – the initiation, propagation and resolution phase, even if the relative importance will vary between epidemics. During the initiation stage, for example, migrants’ adverse working conditions should be considered, especially in the meat and poultry production because it could have a potential role in the initial cross-species transmission for some zoonotic diseases. Barriers to healthcare access and adverse living circumstances, such as overcrowding may play a role in disease propagation, and although usually confined to peer groups, a potential role of transmission to outside populations or even cross-border has been previously described. Conversely, good public health control in these groups will support the resolution of the epidemic. This means that early detection and treatment is not only the right thing to do from a human rights perspective, but also from a public health point of view, especially in COVID-19.
A pre-COVID-19 pandemic analysis of Migration Governance Indicators (MGI) assessments, conducted between 2018 and 2020 and covering 51 countries, showed that there is ample room to improve the inclusion of migrant in national crises plans. According to the analysis, one in five countries has specific measures in place to assist migrants during and after crises, such as internal displacement. However, these crisis plans did not specifically mention measures on maintaining or upscaling health systems during a public health crisis.
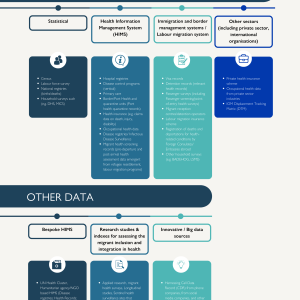
An inclusive approach to epidemic control requires detailed knowledge and information about all relevant population groups, including their demography, their cultural-linguistic and socio-economic needs and of course, their health and illness, including COVID-19. The benefits of ensuring that public health messages can be understood and help appropriately should be obvious for any public health campaign and are vital if COVID-19 is to be successfully controlled. It is also critical to understand potential benefits and costs of public health measures to all population groups, and to avoid inadvertently aggravating vulnerabilities, such as deterrence of health service access through police-enforced social distancing measures or separation of migrants from family and social support networks when being stranded due to border closures.
In many countries, rapidly applied and crude public health measures for COVID-19 are increasingly being fine-tuned in renewed efforts of deconfinement of populations. This phase will require detailed knowledge and information about the epidemic and active inclusion of all migrant population groups in healthcare and in epidemic control plans will not only be the right thing to do from a human rights perspective, but also vital to successful COVID-19 control going forward.
Disclaimer: The opinions expressed in this blog are those of the authors and do not necessarily reflect the views of the International Organization for Migration (IOM) or the United Nations. Any designations employed and the presentation of material throughout the blog do not imply the expression of any opinion whatsoever on the part of IOM concerning the legal status of any country, territory, city or area, or of its authorities, or concerning its frontiers and boundaries.
| Benach J, Muntaner C, Delclos C, Menéndez M, Ronquillo C. | |
| 2011 |
Migration and “Low-Skilled” Workers in Destination Countries. PLOS Medicine. Public Library of Science. 2011; 8:e1001043.
|
| Sadarangani SP, Lim PL, Vasoo S. | |
| 2017 |
Infectious diseases and migrant worker health in Singapore: a receiving country’s perspective. J Travel Med [Internet]. Oxford Academic; 2017 [cited 2020 Apr 24];24.
|
| Liem A, Wang C, Wariyanti Y, Latkin CA, Hall BJ. | |
| 2020 |
The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry. 2020;
|
| Biswas S. | |
| 2020 |
India’s pandemic lockdown turns into a human tragedy. BBC News [Internet]. 2020 Mar 30 [cited 2020 Apr 24]
|
| Wickramage K, Agampodi SB, Mosca D, Peiris S. | |
| 2016 |
Is Sri Lanka prepared for yellow fever outbreaks? A case study. The Lancet Global Health. Elsevier; 2016;4:e909–10.
|
| Chetail * V. | |
| 2017 |
The Human Rights of Migrants in General International Law: From Minimum Standards to Fundamental Rights [Internet]. Migrants and Rights. Routledge; 2017 [cited 2020 Apr 22]. p. 3–34. Available from: https://www.taylorfrancis.com/ |